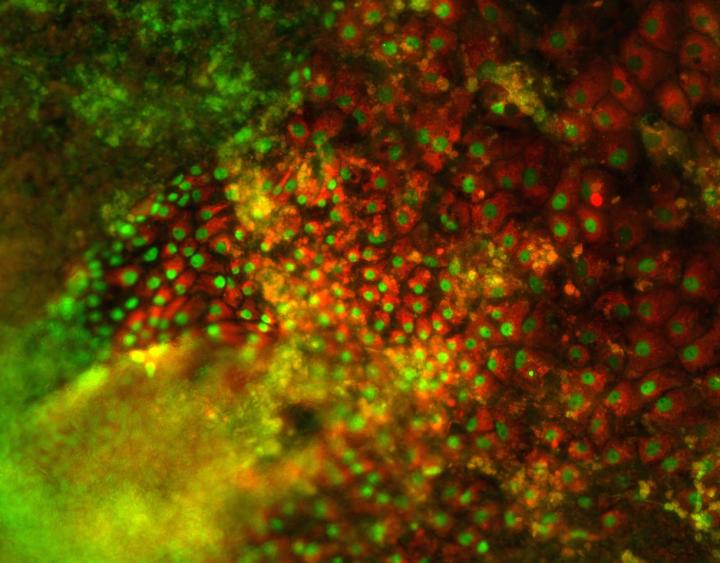
This image shows stem cell-derived hepatocytes emerging. The liver plays a critical role in human metabolism. As the gatekeeper of the digestive track, this massive organ is responsible for drug breakdown and is therefore the first to be injured due to overdose or misuse. Evaluating this drug-induced liver injury is a critical part of pharmaceutical drug discovery and must be carried out on human liver cells. Regretfully, human liver cells, called hepatocytes, are in scarce supply as they can only be isolated from donated organs.
Now, in research published on the cover of the July edition of Hepatology, scientists from the Hebrew University of Jerusalem's Alexander Grass Center for Bioengineering report that they produced large amounts of functional liver cells from human embryonic and genetic engineered stem cells.
"This is quite a revolution for pharmaceutical drug discovery," said Prof. Yaakov Nahmias, the study's senior author. "While other groups have been able to produce liver cells before us, their cells showed little functional activity, and could not be reliably used for drug discovery. In fact, up until now stem cell-derived hepatocytes showed little ability to predict clinical outcome."
The limited availability of functional hepatocytes for drug testing is a major bottleneck bringing pharmaceutical companies to spend $1 billion/year on liver cells alone. "Our ability to produce an unlimited supply of functional liver cells from human pluripotent stem cells can change all that," said Nahmias.
The breakthrough came with the birth of Nahmias' baby girl earlier this year. "I watched her feeding just moments after birth, and realized this is the first time her liver started working," said Nahmias. "Nobody had thought of mimicking this part of human development before, so that's exactly what we did."
The team went on to discover that the bacteria populating the infant gut moments after birth produce vitamin K2 and bile acids that activate the fetal liver's dormant drug metabolism program.
The groundbreaking work further demonstrated that liver cells produced from either embryonic stem cells or genetically engineered skin cells, can detect the toxic effect of over a dozen drugs with greater than 97% accuracy.
"The implications for liver biology and drug discovery are quite staggering," said Prof. Oren Shibolet, Head of the Liver Unit at the Tel-Aviv Sourasky Medical Center, who was not involved in this study. "The method provides access to unlimited amounts of functional liver cells and is likely to critically improve our ability to predict drug toxicity, which was previously limited by the unavailability of liver cells. Furthermore, as gut bacteria develop differently in infants delivered by caesarean section, the mode of delivery can possibly affect newborns' liver maturation. Current practice is to routinely administer Vitamin K to newborns. The data presented suggest that parents abstaining from this practice may cause liver maturation and drug metabolism in their children to develop quiet differently."
Source: The Hebrew University of Jerusalem
 Print Article
Print Article Mail to a Friend
Mail to a Friend
