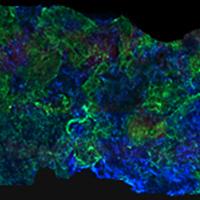
A microscopic image of a 10 mm collagen scaffold containing a uniform distribution of skin cells (blue) seeded on top of a 3-D polylysine gradient (green). Engineers at Georgia Tech have used skin cells to create artificial bones that mimic the ability of natural bone to blend into other tissues such as tendons or ligaments. The artificial bones display a gradual change from bone to softer tissue rather than the sudden shift of previously developed artificial tissue, providing better integration with the body and allowing them to handle weight more successfully. The research appears in the August 26, 2008, edition of the Proceedings of the National Academy of Sciences.
"One of the biggest challenges in regenerative medicine is to have a graded continuous interface, because anatomically that's how the majority of tissues appear and there are studies that strongly suggest that the graded interface provides better integration and load transfer," said Andres Garcia, professor in the George W. Woodruff School of Mechanical Engineering at the Georgia Institute of Technology.
Garcia and former graduate student Jennifer Phillips, along with research technician Kellie Burns and their collaborators Joseph Le Doux and Robert Guldberg, were not only able to create artificial bone that melds into softer tissues, but were also able to implant the technology in vivo for several weeks.
They created the tissue by coating a three-dimensional polymer scaffold with a gene delivery vehicle that encodes a transcription factor known as Runx2. They generated a high concentration of Runx2 at one end of the scaffold and decreased that amount until they ended up with no transcription factor on the other end, resulting in a precisely controlled spatial gradient of Runx2. After that, they seeded skin fibroblasts uniformly onto the scaffold. The skin cells on the parts of the scaffold containing a high concentration of Runx2 turned into bone, while the skin cells on the scaffold end with no Runx2 turned into soft tissue. The result is an artificial bone that gradually turns into soft tissue, such as tendons or ligaments.
If the technology is able to pass further testing, one application could be anterior cruciate ligament (ACL) surgery. Oftentimes, ACL surgery fails at the point where the ligament meets the bone. But if an artificial bone/ligament construct with these types of graded transitions were implanted, it might lead to more successful outcomes for patients.
"Every organ in our body is made up of complex, heterogeneous structures, so the ability to engineer tissues that more closely mimic these natural architectures is a critical challenge for the next wave of tissue engineering," said Phillips, who is now working at Emory University as a postdoctoral research fellow in developmental biology.
Now that they have been able to demonstrate that they can implant the tissue in vivo for several weeks, the team's next step is to show that the tissue can handle weight for an even longer period of time.
Source : Georgia Institute of Technology
 Print Article
Print Article Mail to a Friend
Mail to a Friend
