Investigators at Georgetown University Medical Center have been able to use simple, nontoxic chemical injections to add and remove fat in targeted areas on the bodies of laboratory animals. In what they call a “stunning research advance,” investigators at Georgetown University Medical Center have been able to use simple, non-toxic chemical injections to add and remove fat in targeted areas on the bodies of laboratory animals. They say the discovery, published online in Nature Medicine on July 1, could revolutionize human cosmetic and reconstructive plastic surgery and treatment of diseases associated with human obesity.
Investigators say these findings may also, over the long-term, lead to better control of metabolic syndrome, which is a collection of risk factors that increase a patient’s chances of developing heart disease, stroke, and diabetes. Sixty million Americans were estimated to be affected by metabolic syndrome in 2000, according to a study funded by the Centers for Disease Control in 2004.
In the paper, the Georgetown researchers describe a mechanism they found by which stress activates weight gain in mice, and they say this pathway − which they were able to manipulate − may explain why people who are chronically stressed gain more weight than they should based on the calories they consume.
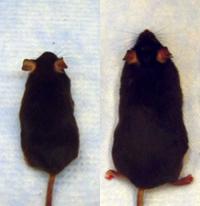
This pathway involves two players − a neurotransmitter (neuropeptide Y, or NPY) and the receptor (neuropeptide Y2 receptor, or Y2R) it activates in two types of cells in the fat tissue: endothelial cells lining blood vessels and fat cells themselves. In order to add fat selectively to the mice they tested, researchers injected NPY into a specific area. The researchers found that both NPY and Y2R are activated during stress, leading to apple-shape obesity and metabolic syndrome. Both the weight gain and metabolic syndrome, however, were prevented by administration of Y2R blocker into the abdominal fat.
“We couldn’t believe such fat remodeling was possible, but the numerous different experiments conducted over four years demonstrated that it is, at least in mice; recent pilot data also suggest that a similar mechanism exist in monkeys as well,” said the study’s senior author, Zofia Zukowska, M.D., Ph.D., professor and chair of the Department of Physiology & Biophysics at Georgetown University Medical Center.
“We are hopeful that these findings might eventually lead to control of metabolic syndrome, which is a huge health issue for many Americans,” she said. “Decreasing fat in the abdomen of the mice we studied reduced the fat in their liver and skeletal muscles, and also helped to control insulin resistance, glucose intolerance, blood pressure and inflammation. Blocking Y2R might work the same way in humans, but much study will be needed to prove that.”
More immediately, the findings could provide some comfort to stressed individuals who blame themselves for a weight gain that seems outsized given the food they eat, said Lydia Kuo, a medical student who earned her Ph.D. in physiology due to work on the study.
“This is the first study to show that stress has a direct effect on fat accumulation, body weight and metabolism,” she said. “In humans, this kind of stress-mediated fat gain may have nothing to do with the brain, and is actually just a physiological response of their fat tissue.”
And perhaps the most rapid clinical application of these results will be in both cosmetic and reconstructive plastic surgery, said co-author Stephen Baker, M.D., D.D.S, associate professor of plastic surgery at Georgetown University Hospital. The ability to add fat as a graft would be useful for facial rejuvenation, breast surgery, buttock and lip enhancement, and facial reconstruction, he said, and using injections like those tested in this study could make fat grafts predictable, inexpensive, biocompatible and permanent.
Equally important, blocking Y2R resulted in local elimination of adipose, or fat, tissue, said Baker. “This is the first well-described mechanism found that can effectively eliminate fat without using surgery,” he said. “A safe, effective, non-surgical means to eliminate undesirable body fat would be of great benefit to our patients.”
Roxanne Guy, MD, president of the American Society of Plastic Surgeons, of which Baker is a member, is also excited by the findings, although she agrees that more research is needed to find out how the animal findings translate in humans. “Providing a long lasting, natural wrinkle filler and a scientifically studied, non-surgical method for melting fat could revolutionize ‘growing old gracefully,’” she said. “This discovery could also have positive implications for reconstructive plastic surgery procedures performed on the face and breasts.”
Stress + “comfort” foods = excess weight gain
As part of the study, Zukowska and her team examined the effect of several forms of chronic stress that mice in the wilderness can encounter, such as exposure for an hour a day over a two-week period to standing in a puddle of cold water or to an aggressive alpha mouse, and they conducted the experiments in combination with a regular diet or with a high-fat, high-sugar diet. Stressed animals fed a normal diet did not gain weight, but stressed mice given a high-fat diet did. In fact, the researchers found these mice put on more weight than expected given the calories they were consuming.
“They gained twice as much fat as would be expected, and it was all in their belly area,” Kuo said. Stressed versus non-stressed animals ate the same amount of food, but the stressed animals processed it differently, she said, explaining, “the novel finding here is that NPY works on fat tissue, not in the brain.”
This finding makes sense if evolutionary advantage is considered, Zukowska said. “If you can store fat for times of hardship, you have a fat reserve that can be turned into energy for the next fight.
“The same mechanism may be happening in humans,” she said. “An accumulation of chronic stressors, like disagreements with your boss, taking care of a chronically ill child, or repeated traffic road rages, could be acting as an amplifier to a hypercaloric diet when protracted over time. Depression may also be acting as a stressor.”
Not only were the stressed mice much fatter, they began to exhibit the metabolic and cardiovascular consequences of obesity, Kuo said. “They had the glucose intolerance seen in diabetes, elevated blood pressure, inflammation in the blood vessels, and fat in their livers and muscles.”
“Although we don’t expect that, in the future, a person will be able to eat everything he or she wants, chase it down with a Y2R blocking agent, and end up looking like a movie star,” said Zukowska, “we are encouraged that these findings could improve human health.”
“The concepts described in this study might give us the tools to design one method to remodel fat and another to tackle obesity and metabolic syndrome,” Baker said. “It is very exciting.”
Source : Georgetown University Medical Center
 Print Article
Print Article Mail to a Friend
Mail to a Friend
